In order to study how skin health and disease are related, researchers had to first understand why disease causes us to experience inflammation. When it comes to physical injuries, inflammation is a necessary part of the healing process because it builds a buffer around the wound to protect it. Even though we try to reduce the swelling around the wound, it’s actually the inflammation that helps the area heal. Once new skin grows around the wound, the inflammation usually subsides on its own.
 Inflammation is characterized by a few mild to severe signs, depending on the nature of the medical condition. When damage to tissue occurs, the first thing most people notice is that the affected area is painful. Chemical compounds are released in the body to stimulate the nerves so pain messages can be delivered to the brain. This prevents you from touching the area, since pain is stronger with physical contact. The area will also appear redder than your normal skin color, because the capillaries in that part of the body are carrying a higher concentration of blood. The increased blood flow will also make the affected area feel hotter and more sensitive.
Inflammation is characterized by a few mild to severe signs, depending on the nature of the medical condition. When damage to tissue occurs, the first thing most people notice is that the affected area is painful. Chemical compounds are released in the body to stimulate the nerves so pain messages can be delivered to the brain. This prevents you from touching the area, since pain is stronger with physical contact. The area will also appear redder than your normal skin color, because the capillaries in that part of the body are carrying a higher concentration of blood. The increased blood flow will also make the affected area feel hotter and more sensitive.
At this point, physical swelling may begin. While this happens to protect the affected area, it also causes a reduction in mobility. The swelling builds a physical barrier that inhibits the free range of motion you usually experience. Trying to push, or force, motion of that area often triggers a more intense sensation of pain.
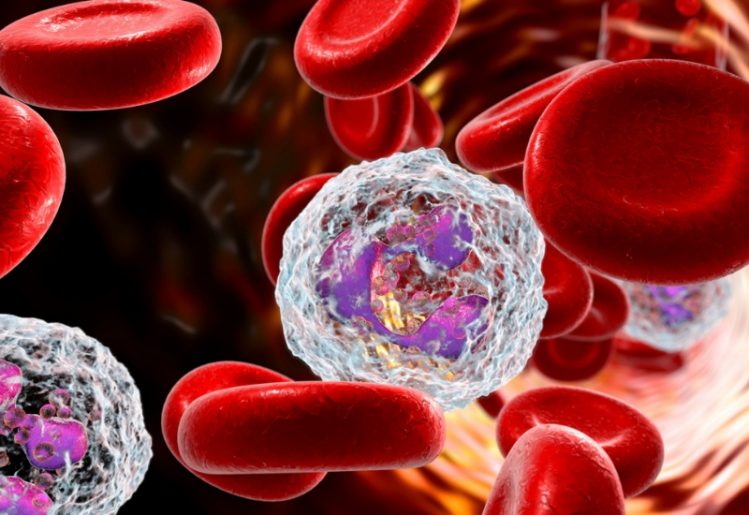
Some people think that inflammation is the result of an infection, but this isn’t necessarily true. What does actually happen is that the smallest arteries in the affected area will enlarge to allow maximum blood flow. This allows the capillaries to move more easily between cells and the blood, attracting proteins as they move through the arteries. Finally, white blood cells called neutrophils are released and they begin consuming the foreign microorganisms in the affected area. This immune response is what triggers inflammation.
Research Uncovers a Connection Between Skin Health and Disease
The skin is the largest organ of the body, so it only makes sense that it plays a major role in how we’re affected by disease. Previous research has found that inflammation of the skin can be linked to diseases like type 2 diabetes, Alzheimer’s disease, osteoporosis and atherosclerosis. As the largest organ in the body, even the smallest levels of inflammation can affect the body in significant ways.
As people age, they experience increased dryness, irritation and itchiness of the skin. Researcher Dr. Mao-Qiang Man believes this to be a sign of inflammation in the body, prompted by heightened cytokines. The cytokines released into the blood supply help younger skin heal more easily, but older, dryer skin is less resilient. As a result, inflammation becomes chronic and the body has more difficulty filtering out pathogens.
In the new study, designed to examine the effects of skin treatments on disease, Dr. Theodora Mauro reveals that skin conditions, particularly psoriasis and dermatitis, can increase the risk of heart disease. If skin health could be restored, Dr. Mauro surmised that inflammation and the risks of disease could also be affected. In this case, keeping skin moisturized might be an effective way of fighting degenerative diseases.
Is Skin Moisturizer an Effective Weapon Against Disease?
 The researchers for the pilot study chose 33 older adults, ranging in ages from 58 to 95. Since cytokines are good indicators of internal inflammation, the researchers started the 30 day study by measuring cytokine levels in each of the participants. Throughout the study, each participant rubbed moisturizer into their skin from head to toe, twice each day.
The researchers for the pilot study chose 33 older adults, ranging in ages from 58 to 95. Since cytokines are good indicators of internal inflammation, the researchers started the 30 day study by measuring cytokine levels in each of the participants. Throughout the study, each participant rubbed moisturizer into their skin from head to toe, twice each day.
There are different types of cytokines that can inhabit the body, but three in particular are responsible for age-related degenerative illnesses. They are tumor necrosis factor alpha, interleukin-1 beta and interleukin-6. When a moisturizer containing ceramides, cholesterol and free fatty acids was applied twice daily, there was a noticeable drop in those cytokine levels. The levels dropped low enough that the participants’ cytokines were similar to those of people in their 30s.
This was the first study of its kind, linking skin health to inflammation and the risks of degenerative illnesses. While it laid the groundwork and established that there is a connection, more research will have to be conducted. As future studies confirm the correlation between disease and skin health, there will likely be greater emphasis placed on keeping skin moisturized and healthy.
Skin health has always been a major concern, particularly in terms of the damage caused by the sun’s rays. In addition to moisturizing twice per day, it’s important to always wear sunscreen outdoors and to avoid direct sunlight at the hottest times of the day. Using a natural supplement designed to nourish the skin from the inside out by delivering crucial nutrients may also be beneficial. A dermatologist can recommend more skin care tips, so you can keep your body’s largest organ healthy and youthful into old age.
 Depression encompasses more than merely feeling down or being unhappy. This condition is a
Depression encompasses more than merely feeling down or being unhappy. This condition is a  In a second study, a group of Belgian biologists found a significant link between an individual’s
In a second study, a group of Belgian biologists found a significant link between an individual’s  The
The  Beyond the findings from Dr. Saji and his team, researchers from the Catholic University of Leuven in Belgium have also found a link between gut bacteria composition and clinical depression. According to the researcher’s findings, published in Nature Microbiology, most of the gut bacteria in our body are able to create neurotransmitters, including dopamine and serotonin. The researchers also figured out that people who have been diagnosed with
Beyond the findings from Dr. Saji and his team, researchers from the Catholic University of Leuven in Belgium have also found a link between gut bacteria composition and clinical depression. According to the researcher’s findings, published in Nature Microbiology, most of the gut bacteria in our body are able to create neurotransmitters, including dopamine and serotonin. The researchers also figured out that people who have been diagnosed with  Chemotherapy holds its ground as the most popular and readily available treatment for treating cancer and tumors, but it has had its criticisms throughout the years. The treatment utilizes a anti-cancer drugs in an attempt to kill off cancer cells, and while proven effective, it does take a toll on the human body and might even harm your brain.
Chemotherapy holds its ground as the most popular and readily available treatment for treating cancer and tumors, but it has had its criticisms throughout the years. The treatment utilizes a anti-cancer drugs in an attempt to kill off cancer cells, and while proven effective, it does take a toll on the human body and might even harm your brain. People who rarely engage in social interaction with others may be harming their brains as well. Failing to meet one’s physical, mental and social needs could lead to
People who rarely engage in social interaction with others may be harming their brains as well. Failing to meet one’s physical, mental and social needs could lead to  Aside from the problems caused by the over-prescription of antibiotics, recent research has uncovered other
Aside from the problems caused by the over-prescription of antibiotics, recent research has uncovered other  In recent years, the
In recent years, the  Recently, a team of University of Tasmania researchers led by Michele Callisaya conducted a study to find out why cognitive decline is prevalent in people with type 2 diabetes. The project looked at 705 adults between the ages of 55 and 90. The testing included brain size measurements as well as cognition evaluations.
Recently, a team of University of Tasmania researchers led by Michele Callisaya conducted a study to find out why cognitive decline is prevalent in people with type 2 diabetes. The project looked at 705 adults between the ages of 55 and 90. The testing included brain size measurements as well as cognition evaluations. Increasing the amount of
Increasing the amount of