Do you suffer from a chronic medical condition? If so, this review of the advancements in chronotherapy may prepare you to better advocate for your healthcare.
For generations, people have been saying that timing is everything. In recent years, breakthroughs in healthcare have brought a whole new meaning to this old saying that affects not only our daily routines, but most importantly, our overall health.
Chronotherapy and the Circadian Rhythm
Although not a new concept, the use of chronotherapy is steadily expanding. Chronotherapy, a subset of chronobiology, is the science of delivering medications and therapies in harmony with the circadian rhythms of the body and of certain diseases. Today, various treatments continue to be administered to coincide with our body’s internal clocks for optimal outcomes.
Circadian rhythms control fluctuations in the chemistry of our body hourly, daily and seasonally. Endogenous in nature, the circadian rhythm is influenced by signals within our environment including light, temperature and food intake. These signals tailor the circadian rhythm into a predictable 24-hour pattern.
Disease-Specific Circadian Rhythms
Just as every person’s body has its own circadian rhythms, so do certain diseases. Extensive research shows that the diseases that follow patterns of circadian rhythm can have improved outcomes, as treatment with chronotherapy can positively influence the manner in which they are managed.
Having knowledge of the circadian rhythms of specific diseases allows healthcare providers to utilize chronotherapy for better treatment outcomes, as drugs can be administered during time periods that will provide the best symptom management.
The extensive research on circadian rhythms and chronotherapy has revealed a great deal of information that is beneficial to the management and treatment of certain diseases. The findings specific to arthritis, bronchial asthma and cardiovascular disorders will be explored.
Arthritis
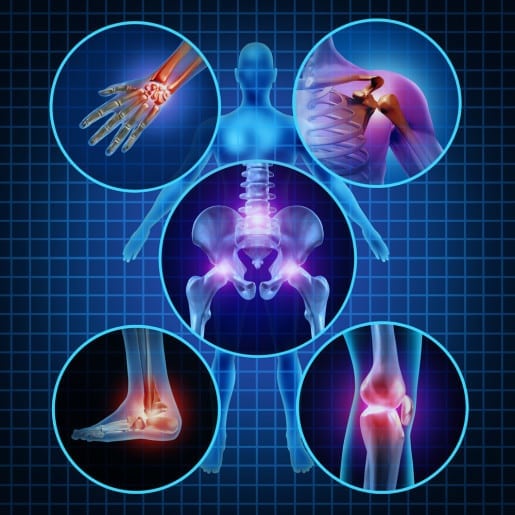 Both rheumatoid arthritis (RA) and osteoarthritis follow their own circadian rhythm. The Journal of Global Trends in Pharmaceutical Sciences reveals a study that suggests chronotherapy for all types of arthritis using non-steroidal anti-inflammatory drugs (NSAIDs) should be timed to ensure the highest drug levels in the blood coincide with an individual’s peak pain levels.
Both rheumatoid arthritis (RA) and osteoarthritis follow their own circadian rhythm. The Journal of Global Trends in Pharmaceutical Sciences reveals a study that suggests chronotherapy for all types of arthritis using non-steroidal anti-inflammatory drugs (NSAIDs) should be timed to ensure the highest drug levels in the blood coincide with an individual’s peak pain levels.
People who suffer from RA are more likely to experience joint pain and finger swelling during the morning hours. Those with osteoarthritis have less pain during the morning compared to the rest of the day. Many arthritis sufferers rely on NSAIDs for pain relief, but because they can have bothersome side effects, the timing of administration is not only important for their effectiveness, but in reducing the risk of side effects as well.
As symptoms of RA are worse in the morning, the administration of long-acting NSAIDs such as ketoprofen, indomethacin and flubiprofen at bedtime provides the maximum therapeutic effect and minimizes their side effects.
Certain mechanisms of RA, including higher cortisol levels during the day and pro-inflammatory conditions during the night related to elevated levels of prolactin and melatonin, have led researchers to believe that a practical approach to managing this debilitating disease would be the chronotherapeutic use of corticosteroids to increase their efficacy and reduce the risk of adverse events.
One scientific report references a study performed by Buttgereit and co-workers, which highlights the clinical relevance of the chronotherapeutic use of glucocorticoid therapy in low doses for RA suppression, as morning stiffness can be effectively reduced by an evening dose of a modified-release prednisone tablet.
Bronchial Asthma
Compared to other diseases, asthma has more circadian variations. While studying the circadian rhythm associated with asthma, researchers determined the lung function of even healthy individuals dips during the early morning hours; a phenomenon that’s more pronounced in those with asthma. The decrease in lung function can be significant, between 25 to 50 percent.
Also, airway resistance in asthmatic individuals increases progressively during the night, leading to frequent awakenings and sleep disturbances. According to the Journal of Global Trends in Pharmaceutical Sciences, the risk of having an asthma attack is 100-fold greater during the night than during daytime hours.
Upon reviewing data from several clinical studies, researches introduced a proposed chronotherapeutic approach to the management of nocturnal asthma, which is as follows:
- In the morning – Use of a long-acting beta agonist, such as salmeterol (serevent). Studies found that asthma patients who were administered salmeterol in the AM had a significantly-reduced percentage of night awakenings and their lung function was significantly increased.
- At 3 p.m. – Use of an oral corticosteroid.
- Between 6-7 p.m. – Use of sustained-release theophylline. Researchers advise that an individual’s period of wakefulness should be considered with this chronotherapeutic approach, as the pharmacokinetics of theophylline can be altered in those that work the night shift.
- At bedtime – Use of a leukotriene modifier, such as montelukast (singulair).
Cardiovascular Disorders
![]()
 Several functions of the cardiovascular system follow a circadian rhythm, including heart rate, blood pressure, platelet aggregation, blood flow and cardiac output.
Several functions of the cardiovascular system follow a circadian rhythm, including heart rate, blood pressure, platelet aggregation, blood flow and cardiac output.
Upon waking in the morning, heart rate and blood pressure are high with a rise in systolic blood pressure by 20-25 mmHg and diastolic blood pressure by 10-15mmHg. This hypertensive state in the morning is a physiological condition described as the morning surge.
Several trials have been conducted exploring the chronotherapy of hypertension, which has established that changing the time of a treatment, rather than the combination of the treatment, may be a better approach to controlling blood pressure. Their reasoning is related to findings that blood pressure is reported to be highest in the mid-morning, progressively falling throughout the day with the lowest blood pressure to be noted at 3 a.m.
In the morning, the release of cortisol and catecholamine is high. There is also an increase in platelet aggregation. For these reasons, more myocardial infarctions are believed to occur in the morning, with 34 percent taking place between the hours of 6 a.m. and 12 noon.
Other Disorders Governed by Circadian Rhythms
There are other significant medical conditions that follow circadian rhythms as well. Treatment with chronotherapy is expanding. However, not all healthcare providers are on board with this concept yet. The purpose of this article is by no means to provide medical advice, but people who have poorly-managed medical conditions should be aware that additional treatment methods may be available so they can better advocate for their healthcare.
Other significant medical conditions that follow circadian rhythms include:
- Glaucoma
- Innate immunity
- Diabetes
- Epilepsy
- Gastric ulcers
- HIV/AIDS
- Pain
- Cancer
- Allergic rhinitis